On May 26, the Interagency Gender Working Group (IGWG) convened the “Spring Dialogues: IGWG Members Lead the Conversation!” virtual event, the first time IGWG members from around the world directed the discussion at an IGWG event. The Spring Dialogues focused on priority topics and technical challenges identified by IGWG members in the 2021 IGWG Member Survey, with volunteers from India and Nigeria facilitating discussion groups. The event’s objectives were:
- To exchange ideas, experiences, and lessons learned among IGWG members and colleagues working on the ground to tackle common challenges in health programming while advancing gender equality.
- To dialogue with the IGWG community on key issues of interest as identified by members in the 2021 IGWG Member Survey.
- To provide an opportunity for IGWG members from around the world to lead interactive discussions.
Below we share key questions and takeaways from the discussion groups.
Supporting Gender-Transformative Approaches in Adolescent-Focused Programs
Facilitator: Sushmita Mukherjee, Director, Gender and Adolescent Girls, Project Concern International, India
Which social norms were really challenging? How can we make approaches gender-transformative?
- Engage stakeholders (including religious and traditional leaders) early on to get their buy-in.
- Increase childcare options so women can attend health centers.
What are some gender-transformative models across the globe?
- Work with very young adolescents to change norms, to give them a voice (as they often are told to remain silent), and to make them feel comfortable discussing issues that impact them. An example of an adolescent-targeted approach is creating youth clubs.
- Work with couples, such as parents, to discuss healthy relationships; their insights can inform young people and encourage them to participate in adolescent groups.
What has been your experience working across the world with how young people are affected by COVID-19?
- There is a whole ecosystem on WhatsApp, particularly groups of young professionals, trying to help fix the public health system. Groups support one another in finding medical care and sharing resources.
The group also discussed ways to address community backlash against efforts to advance gender equality (e.g. girls’ groups), such as having mentors meet with families of young people, speaking with couples together, and engaging boys and young men early to prevent behaviors that could lead to violence.
Recommended Resources:
- Save the Children’s Gender Roles, Equality, and Transformation (GREAT) Toolkit
- Promundo’s male engagement strategies and programs
- Advancing Learning and Innovation on Gender Norms (ALIGN)
Effectively Advocating for Gender-Transformative Change Within Our Public Health Institutions
Facilitator: Amy Oyekunle, Independent Consultant with expertise on girls and gender-related program design, Nigeria
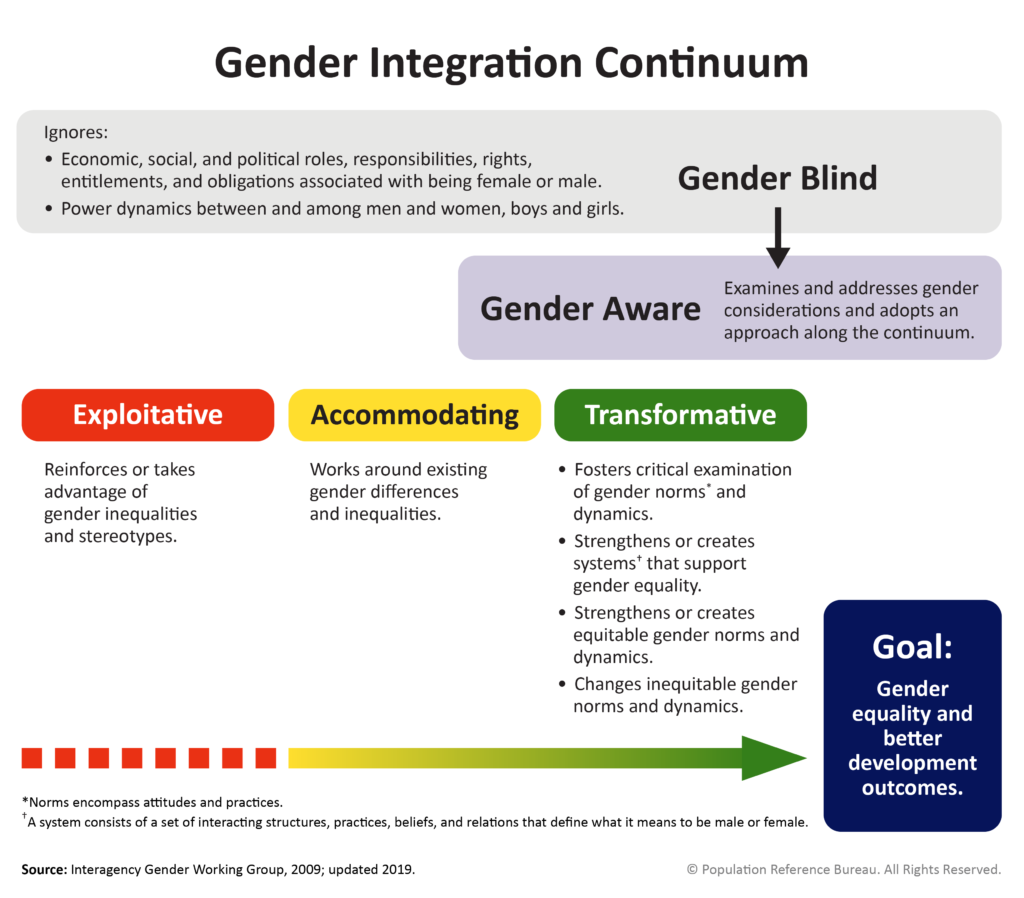
What does “gender-transformative approaches” mean to you?
- Addressing gender norms that make it difficult for someone to be in position that brings them satisfaction and that provides them equal pay. For example, teachers are paid less than they should be because teaching is a “feminine” occupation.
- Organizations taking steps to identify barriers to women’s advancement in leadership positions and their active engagement within organizations, as well as the different obligations that women and men have outside work that impact workplace advancement (e.g., during COVID-19, caring for children and family members has disproportionately affected women).
What types of gender-transformational change would you like to see within your organization?
- Organizational or policy change (e.g., providing parental leave and childcare) alone does not change unrealistic work expectations or community norms or address barriers in societies and cultures. People have to act on change.
- Greater transparency in using data to help people identify economic opportunities (e.g., how many women are receiving loans from the bank).
How can we be effective advocates for gender-transformational change within our organizations?
- We should emphasize the importance of organizations being open to hearing things from their employees that they might not want to hear.
- People need to see the daily impact of harmful gender roles on their lives (such as poor health outcomes, unequal pay, imbalanced time spent on domestic work and childcare, violence, etc.). Change requires positive deviants; it’s all of us as gender champions pointing things out, using data, and applying social pressure to show the negative impacts of gender inequality and help others understand why it’s important.
What are the barriers that might hinder us from being effective advocates and how can we overcome them?
- COVID has shown alternative ways to structure workplaces and to ensure access to childcare and transportation.
- There is strength in numbers. People are more likely to respond to a group than one person and allowing groups to advocate for change helps mitigate backlash against a particular individual—this is transformational.
Supporting Health Care Providers to Better Respond to Gender-Based Violence (GBV)
Facilitator: Oluseyi Olorunfemi, Senior Gender Mainstreaming and Knowledge Management Officer, Centre for Integrated Health Programs, Nigeria
How can we establish effective referral networks between health providers and GBV-specific services?
- Broad stakeholder engagement to establish referral networks and sensitization of professional staff, such as health care providers and law enforcement, as well as their close collaboration with local, trusted NGOs, is key for providing smooth referrals and to ensure services meet the needs of survivors of GBV.
- The ABAAD Resource Center for Gender Equality shared their experience of moving to remote counseling and providing referrals to continue services during the pandemic.
How can we ensure self-care for providers who work with GBV cases?
- Health care providers take care of others but may fail to take care of themselves and seek the needed mental, psychological, emotional, etc. support.
- Self-care is about more than individual responsibility to de-stress; it’s also about the institution providing enough systemic support to those who are doing the hard job of engaging with clients who experience GBV. Institutions must establish policies and practices that support their staff, such as confidential and private counseling, mentorship programs, staff debrief sessions, time off, skill-building for de-stressing, institutional policies that supports all of the above, and supervisors who reinforce the need for self-care.
- Some health care institutions use a screening tool for provider burnout and the results are discussed with leadership to advocate for support systems.
Recommended Resources: